Tests, scans, and diagnosis
Aneurysms are usually detected with CTA or MRA, and sometimes confirmed/treated using catheter angiography (DSA). After suspected rupture, non‑contrast CT is typically first.
When to suspect rupture (aSAH)
Classic features include sudden severe headache (thunderclap), collapse, meningism (neck stiffness), vomiting, or altered consciousness. Some patients report a prior “sentinel” headache days earlier.
Initial evaluation commonly includes:
- Non‑contrast CT head (best early test for blood)
- If CT is negative but suspicion remains: lumbar puncture for xanthochromia (protocol varies)
- Once SAH is confirmed: CTA or DSA to locate the aneurysm
Finding an unruptured aneurysm
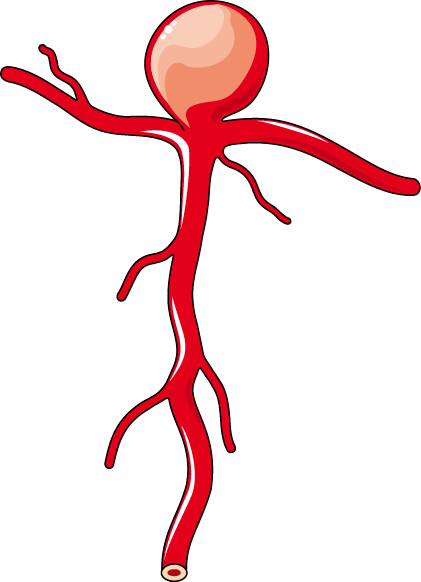
Common shapes (very simplified)
Saccular (“berry”) aneurysms are the most common intracranial type. They arise at branch points and look like a rounded outpouching.
Fusiform aneurysms are elongated dilatations of the vessel segment. In the brain, these are less common and often managed differently.

Illustrations: SMART‑Servier Medical Art (CC BY‑SA / CC BY), via Wikimedia Commons.
Many aneurysms are discovered incidentally during imaging for headaches, dizziness, trauma, or unrelated concerns.
Common tests:
- MRA (MR angiography): no ionizing radiation; may avoid iodinated contrast
- CTA (CT angiography): fast, widely available, high spatial resolution
- DSA (digital subtraction angiography): invasive catheter angiography; best detail; small stroke risk
Imaging modalities (at a glance)
| Test | Strengths | Limitations / risks | Typical use |
|---|---|---|---|
| CT head (non‑contrast) | Fast; excellent for acute blood early after rupture | Radiation; sensitivity declines with time | First test for suspected SAH |
| CTA | Fast; good for aneurysm detection and anatomy | Radiation + iodinated contrast; small lesions can be missed | Workup of suspected aneurysm; planning |
| MRA | No ionizing radiation; useful for follow‑up | May be less sensitive for very small aneurysms; motion artifacts; MRI contraindications | Screening and surveillance |
| DSA | Gold‑standard spatial/temporal resolution; can treat at same sitting | Invasive; contrast; small risk of stroke/complication | Definitive evaluation; pre‑treatment planning; endovascular therapy |
Guidelines and expert reviews describe CTA, MRA, and DSA as complementary tools; choice depends on question (detection vs planning vs follow‑up) and patient factors.
Diagnosis “extras” that influence management
- Exact measurements (max dome size, neck width, aspect ratio)
- Location (anterior vs posterior circulation; posterior often higher rupture risk)
- Morphology (irregularity, blebs/daughter sacs)
- Multiplicity (20–30% of adults with UIA may have more than one aneurysm)
- Growth on surveillance imaging (strong warning sign)