Chance of rupture if an aneurysm is discovered
Rupture risk is not “one number.” It depends on aneurysm size, location, prior rupture history, blood pressure, smoking, age, and imaging features (growth, irregular shape).
Size & location are major drivers
Scores (e.g., PHASES) estimate 5‑year risk
Growth / symptoms often trigger treatment
Typical patterns
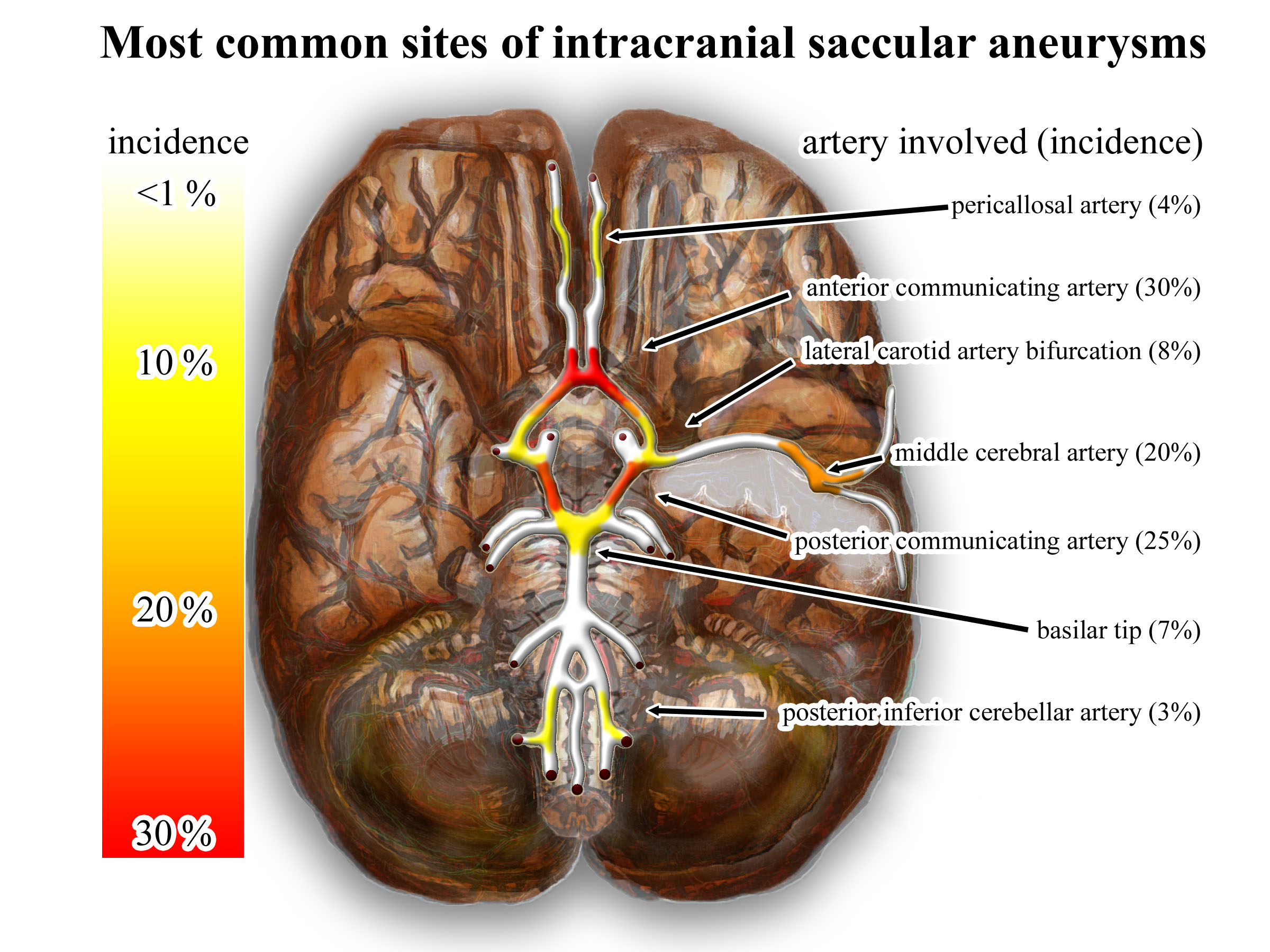
Common sites of saccular aneurysms are clustered around the circle of Willis (anterior communicating, posterior communicating, MCA bifurcation, basilar tip). Location matters because it influences both rupture risk and treatment approach.
Image: Nicholas Zaorsky, CC BY‑SA 3.0 (Wikimedia Commons).
- Small (<7 mm), anterior‑circulation aneurysms without prior SAH often have a low annual rupture risk in large cohort data.
- Posterior circulation (basilar, vertebral, posterior communicating) and larger aneurysms carry higher risk.
- Prior aneurysmal SAH increases the chance another aneurysm will rupture.
- Growth on follow‑up imaging and irregular shape suggest instability.
Decision making is individualized: a low‑risk aneurysm may be safely monitored, while a moderate‑risk aneurysm in a young, otherwise healthy patient may be treated electively.
PHASES concept (5‑year risk estimate)
PHASES is a commonly referenced model using:
- Population (Finnish/Japanese vs other)
- Hypertension
- Age
- Size
- Earlier SAH from another aneurysm
- Site (location)
Clinicians use this alongside anatomy, wall imaging (where available), patient factors, and experience.
Rupture risk: what tends to increase it?
| Factor | Why it matters | How it changes management |
|---|---|---|
| Increase in size (growth) | Growth is a strong surrogate for instability | Often shifts toward treatment (if feasible) |
| Larger size | Higher wall stress and higher observed rupture rates | Treatment more likely recommended |
| Posterior circulation / PCom | Higher rupture risk in multiple cohorts | Lowers size threshold for treatment |
| Irregular morphology (blebs) | Suggests focal weakness and unstable biology | Supports intervention if overall risk acceptable |
| Smoking / uncontrolled hypertension | Promotes formation, growth, and rupture | Intensify risk-factor control; may influence threshold to treat |
| Prior aneurysmal SAH | Higher baseline risk of rupture in remaining aneurysms | More proactive management and surveillance |
A practical way to think about the trade‑off
For an unruptured aneurysm, clinicians compare:
- Natural history risk: probability of rupture over the next 5–10 years (and lifetime)
- Procedural risk: chance of stroke/death/disability from clipping or endovascular therapy
- Durability: likelihood of long‑term occlusion vs need for retreatment (often higher retreatment rates after coiling vs clipping for some anatomies)
Aneurysm size alone is not enough. A 4–6 mm aneurysm can still rupture, but the average risk is generally lower; clinicians look for additional risk signals (location, shape, growth, symptoms).
Search within this page